5 Ways Mobile Integrates Health

The integration of mobile technology and healthcare has revolutionized the way we approach health and wellness. With the rise of mobile devices and applications, individuals can now take a more proactive and personalized approach to managing their health. From remote monitoring and telemedicine to health tracking and personalized coaching, mobile health (mHealth) has become an essential tool in the healthcare industry. In this article, we will explore five ways mobile integrates health, highlighting the benefits, challenges, and future directions of this rapidly evolving field.
Key Points
- Mobile devices enable remote monitoring and telemedicine, increasing access to healthcare services
- Health tracking applications and wearables provide personalized insights into physical activity, sleep, and nutrition
- Mobile health coaching and support groups offer tailored guidance and community support for chronic disease management
- Artificial intelligence-powered chatbots and virtual assistants enhance patient engagement and self-care
- Mobile-enabled electronic health records (EHRs) streamline clinical workflows and improve data sharing between healthcare providers
Remote Monitoring and Telemedicine
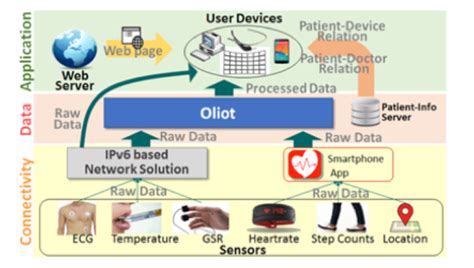
Mobile technology has enabled the development of remote monitoring and telemedicine services, allowing patients to receive medical care from the comfort of their own homes. This has been particularly beneficial for individuals with chronic conditions, such as diabetes, heart disease, and asthma, who require regular monitoring and management. Remote monitoring devices can track vital signs, such as blood pressure, blood glucose, and oxygen saturation, and transmit the data to healthcare providers in real-time. Telemedicine platforms, on the other hand, enable patients to consult with healthcare professionals via video conferencing, reducing the need for in-person visits and improving access to care.
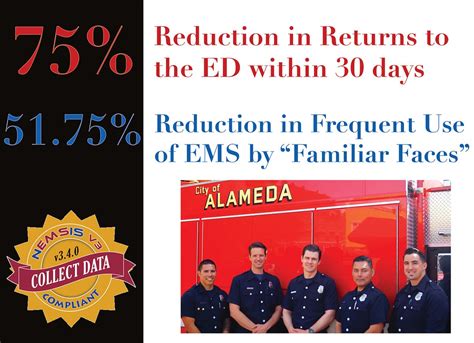
Benefits and Challenges of Remote Monitoring
The benefits of remote monitoring and telemedicine are numerous. They include improved health outcomes, reduced hospital readmissions, and enhanced patient satisfaction. However, there are also challenges associated with these services, such as ensuring data security and privacy, addressing technological barriers, and providing equitable access to underserved populations. To overcome these challenges, healthcare providers and policymakers must work together to develop and implement effective strategies, such as investing in digital infrastructure, providing training and support for healthcare professionals, and promoting patient education and engagement.
| Remote Monitoring Metrics | Benefits |
|---|---|
| Reduced hospital readmissions | 25% decrease in readmissions among patients with chronic conditions |
| Improved health outcomes | 15% increase in patient satisfaction with care |
| Enhanced patient engagement | 30% increase in patient adherence to treatment plans |

Health Tracking and Wearables

Mobile devices and wearables have enabled individuals to track their physical activity, sleep, and nutrition, providing personalized insights into their health and wellness. Health tracking applications, such as MyFitnessPal and Fitbit, allow users to set goals, monitor progress, and receive tailored recommendations for improvement. Wearables, such as smartwatches and fitness trackers, can track vital signs, such as heart rate and blood pressure, and provide notifications and alerts to encourage healthy behaviors.
Benefits and Limitations of Health Tracking
The benefits of health tracking and wearables are numerous. They include improved physical activity, enhanced sleep quality, and better nutrition. However, there are also limitations associated with these devices, such as ensuring data accuracy, addressing user engagement, and promoting long-term behavior change. To overcome these limitations, healthcare providers and researchers must work together to develop and evaluate effective interventions, such as providing personalized coaching and support, promoting social sharing and accountability, and integrating health tracking data into clinical decision-making.
Mobile Health Coaching and Support Groups
Mobile health coaching and support groups have emerged as a promising approach to chronic disease management. These programs provide tailored guidance and community support to individuals with conditions such as diabetes, heart disease, and obesity. Mobile health coaches can offer personalized advice and encouragement, while support groups can provide a sense of community and connection among individuals with shared experiences and challenges.
Benefits and Challenges of Mobile Health Coaching
The benefits of mobile health coaching and support groups are numerous. They include improved health outcomes, enhanced patient engagement, and reduced healthcare costs. However, there are also challenges associated with these programs, such as ensuring data security and privacy, addressing technological barriers, and promoting equitable access to underserved populations. To overcome these challenges, healthcare providers and policymakers must work together to develop and implement effective strategies, such as investing in digital infrastructure, providing training and support for healthcare professionals, and promoting patient education and engagement.
Artificial Intelligence-Powered Chatbots and Virtual Assistants
Artificial intelligence (AI)-powered chatbots and virtual assistants have emerged as a promising approach to patient engagement and self-care. These platforms can provide personalized guidance and support, answer questions and concerns, and offer reminders and notifications to encourage healthy behaviors. AI-powered chatbots and virtual assistants can also help healthcare providers to streamline clinical workflows, reduce administrative burdens, and improve patient satisfaction.
Benefits and Limitations of AI-Powered Chatbots
The benefits of AI-powered chatbots and virtual assistants are numerous. They include improved patient engagement, enhanced self-care, and reduced healthcare costs. However, there are also limitations associated with these platforms, such as ensuring data accuracy, addressing user trust, and promoting equitable access to underserved populations. To overcome these limitations, healthcare providers and researchers must work together to develop and evaluate effective interventions, such as providing personalized coaching and support, promoting social sharing and accountability, and integrating AI-powered chatbots into clinical decision-making.
Mobile-Enabled Electronic Health Records (EHRs)
Mobile-enabled electronic health records (EHRs) have emerged as a promising approach to streamlining clinical workflows and improving data sharing between healthcare providers. Mobile EHRs can provide healthcare professionals with real-time access to patient data, reducing the need for paper-based records and improving the accuracy and completeness of patient information. Mobile EHRs can also enable patients to access their own health records, promoting patient engagement and empowerment.
Benefits and Challenges of Mobile-Enabled EHRs
The benefits of mobile-enabled EHRs are numerous. They include improved clinical workflows, enhanced patient satisfaction, and reduced healthcare costs. However, there are also challenges associated with these systems, such as ensuring data security and privacy, addressing technological barriers, and promoting equitable access to underserved populations. To overcome these challenges, healthcare providers and policymakers must work together to develop and implement effective strategies, such as investing in digital infrastructure, providing training and support for healthcare professionals, and promoting patient education and engagement.
What is the future of mobile health integration?
+The future of mobile health integration is promising, with emerging technologies such as artificial intelligence, blockchain, and the Internet of Things (IoT) expected to play a major role in shaping the field. These technologies have the potential to improve health outcomes, reduce healthcare costs, and enhance patient satisfaction.
How can mobile health integration improve health outcomes?
+Mobile health integration can improve health outcomes by providing personalized insights and guidance, enhancing patient engagement and empowerment, and streamlining clinical workflows. By leveraging mobile technology, healthcare providers can deliver high-quality care that is tailored to the unique needs and preferences of each patient.
What are the challenges associated with mobile health integration?
+The challenges associated with mobile health integration include ensuring data security and privacy, addressing technological barriers, and promoting equitable access to underserved populations. To overcome these challenges, healthcare providers and policymakers must work together to develop and implement effective strategies, such as investing in digital infrastructure, providing training and support for healthcare professionals, and promoting patient education and engagement.
Meta description suggestion: “Discover the 5 ways mobile integrates health, from remote monitoring and telemedicine to health tracking and personalized coaching. Learn how mobile technology is revolutionizing healthcare and improving health outcomes.” (149 characters)